she lived in two countries,
waffling between fear and joy.
joy in having one more day but
fear in being one day closer to the grave.
she analyzed every change in her health
with the scrutiny of a true professional.
she asked questions like,
"can things go bad really fast?"
"is this the end?"
in spite of the doubts and struggles,
she threw herself into living life with gusto.
she truly embraced the joy that overshadowed
the clouds of questions that swarmed around her.
she made living with terminal cancer look easy.
in fact, she made it look so easy that people
forgot she was dying.
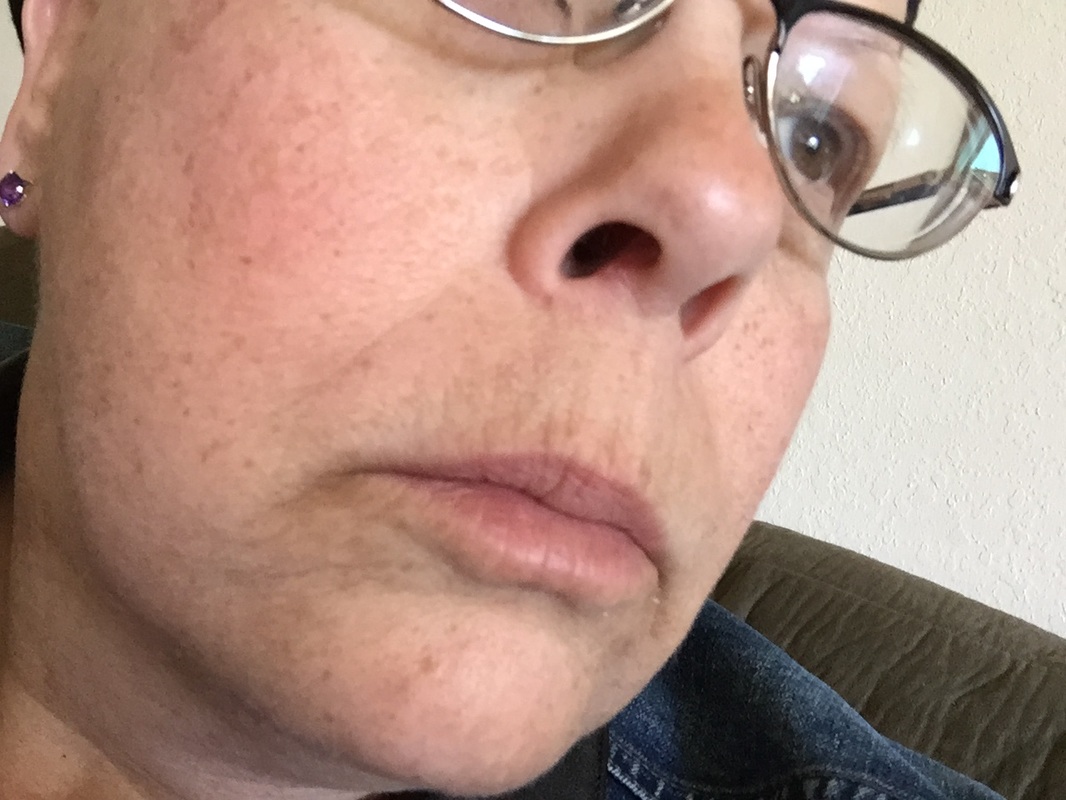
she repeatedly heard comments about how
great she looked.
she made living with a terminal illness look normal.
there's nothing normal about living with disease.
those with early stage diagnoses are often cheered
when they complete 4, 6, 8, or 12 chemotherapy treatments.
cheers are given at the end of a year of herceptin.
there are no cheers for the terminal patient,
although there is incredible encouragement.
people are hard-pressed to understand what it
means to endure 1,250 days of non-stop treatments.
and then she died at age 32.
we're all left wondering how this could be.
in spite of our own lives with this disease,
we all forget how sick we really are.
we'll attend her funeral where we'll hear everyone saying,
"but she was doing so well!"
"i had no idea she was so sick!"
"i can't believe she's gone!"
that's the insidiousness of the disease.
we go on, day after day, month after month,
year after year.
if we're lucky, those years stretch beyond average
expectations.
we live each day with joy,
grateful for each one.
we try not to live in fear of the grave
looming off in the distance.







 RSS Feed
RSS Feed
